Pain shoots down your leg like lightning. Your buttock throbs. Walking feels wrong. You know something’s off, but what exactly? Two sneaky conditions love to masquerade as each other: piriformis syndrome vs sciatica. They both mess with your leg, create similar aches, and leave you guessing. But here’s the thing – they come from totally different places and need completely different fixes. You could spend months chasing the wrong treatment.
In this article, we’ll break down how sciatica vs piriformis syndrome differ, what tests can tell them apart, and which treatments work for each condition. You’ll learn simple ways to spot the signs, understand what causes each problem, and know when to get professional help. By the end, you’ll have the tools to figure out what’s really going on with your pain.
What is Sciatica?
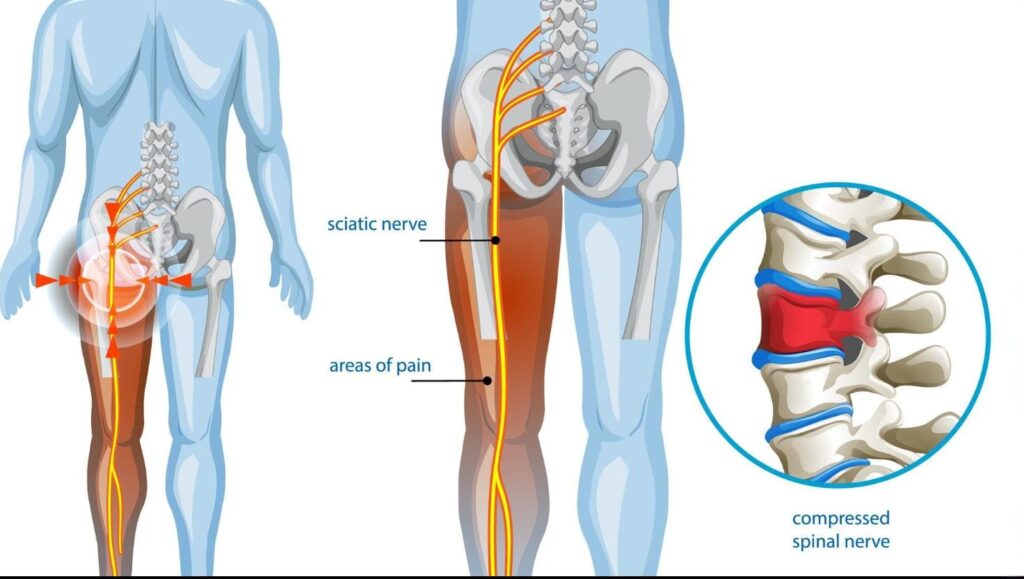
Sciatica is pain that happens when something squeezes your sciatic nerve. Think of this nerve like a thick electrical cable that runs from your lower back down through your leg to your toes. Your sciatic nerve is huge – about as thick as your thumb. It carries messages between your brain and your leg muscles. When something presses on this nerve, it sends pain signals shooting down your leg.
What squeezes the nerve? Usually, problems in your spine. A disc might bulge out like a flat tire, pressing on the nerve. Your spine might get narrow spots that pinch nerves. Bone spurs can grow and poke at nerve tissue. Sometimes one back bone slides forward over another, trapping nerves. Think of it like stepping on a garden hose – the water (nerve signals) can’t flow properly, so you get backup problems downstream.
What Does Sciatica Feel Like?
Sciatica pain feels like an electric shock running down your leg. Some people describe it as burning or sharp shooting pains that make them gasp. The pain starts in your lower back or buttocks, then travels down one leg. Real sciatica often goes past your knee, sometimes all the way to your foot. It’s like the pain follows a map down your leg.
You might also get:
- Numbness that makes parts of your leg feel dead
- Tingling like your foot fell asleep
- A weakness that makes you stumble
Certain things make it worse:
- Sitting too long (like at your desk)
- Coughing or sneezing
- Bending forward
- Standing for hours
For example, many office workers notice their sciatica flares up after long meetings or when they laugh hard.
What is Piriformis Syndrome?
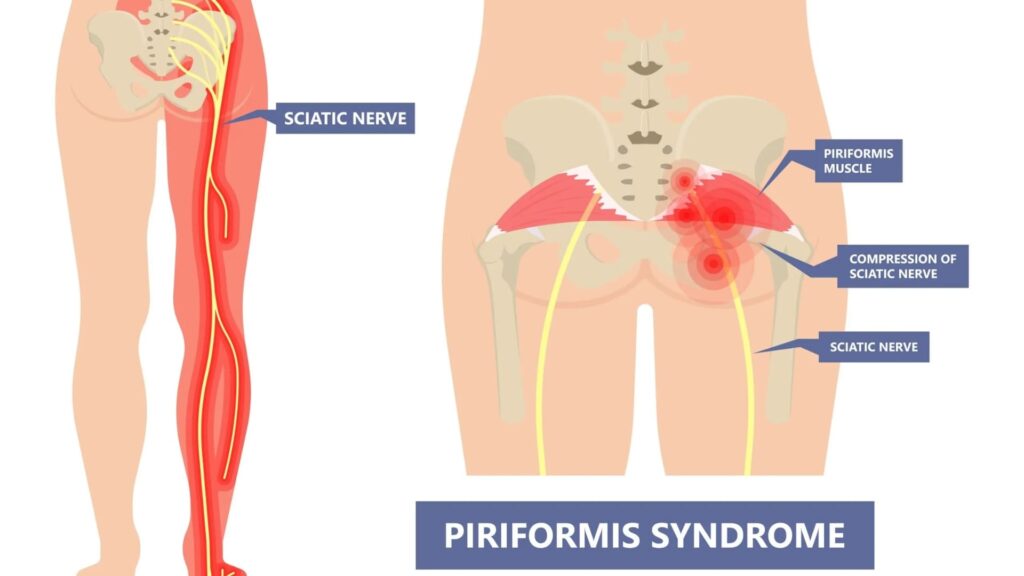
Piriformis syndrome happens when a small muscle in your buttock squeezes your sciatic nerve. The piriformis muscle sits deep under your bigger butt muscles. Its job is to help rotate your hip. Here’s the problem: your sciatic nerve runs right next to this muscle. In some people, the nerve actually goes through the muscle. When the piriformis gets tight or swollen, it squeezes the nerve like a clamp.
What irritates the piriformis?
- Sitting on hard surfaces for hours (like truck drivers)
- Running or cycling a lot
- Falling on your butt
- Having tight hip muscles from sitting too much
Think of it like wearing a belt that’s too tight – it pinches what’s underneath.
How long does piriformis syndrome last? Most people feel better in 2-6 weeks with the right treatment. But if you ignore it, you might deal with pain for months.
What Does Piriformis Syndrome Feel Like?
Piriformis syndrome pain sits deep in your buttock like a constant ache. People often say it feels like sitting on a golf ball. The pain might travel down the back of your thigh, but it rarely goes past your knee. Your buttocks are the main problem area. You might get some numbness or tingling, but it usually stays in your buttocks and upper thigh, not your whole leg, like with sciatica.
What makes it worse:
- Sitting (especially on hard chairs)
- Climbing stairs
- Running
- Twisting your hip inward
For example, many people first notice piriformis syndrome after a long car trip or when they start a new exercise routine. Understanding these patterns helps you take the first step toward effective pain management that targets your specific problem.
Sciatica vs Piriformis Syndrome: Drawing the Clear Lines
Time to separate these two troublemakers. Sciatica vs piriformis syndrome comes down to some key differences that, once you know them, make things much clearer.
| Comparison Factor | Sciatica (Spinal Origin) | Piriformis Syndrome |
|---|---|---|
| Source of the Problem | Spine: discs, bones, or other spinal structures pressing on nerve roots | Buttock muscle (piriformis) squeezing the sciatic nerve |
| Primary Pain Location | Lower back radiating down entire leg, often to foot/toes | Buttock with possible radiation to mid-thigh (rarely below knee) |
| Pain Quality | Sharp, shooting, electric shock-like, burning | Deep ache in the buttock, sometimes sharp, like sitting on a golf ball |
| Aggravating Factors | Spine movements: bending forward, coughing, sneezing, prolonged sitting | Hip movements: sitting, climbing stairs, running, inward leg rotation |
| Neurological Symptoms | Widespread numbness/tingling, possible foot drop, muscle weakness | Limited numbness/tingling mainly in the buttocks and upper thigh |
| Progression Pattern | Often, gradual worsening occurs as spinal problems advance | More erratic – varies with activity levels and muscle tension |
| Response to Movement | Often worse with spinal flexion, better with extension | Often worse with hip flexion, better with stretching |
Understanding these differences helps crack the piriformis syndrome vs sciatica code, though you’ll still need professional eyes on the problem for a definitive answer.
How to Differentiate Sciatica from Piriformis Syndrome?
Self-diagnosis only gets you so far. These conditions can overlap, and other problems can mimic both. Professional evaluation cuts through the guesswork and gets you real answers.
What to Expect at the Doctor’s Office?
Your doctor becomes a detective, gathering clues about your pain. They’ll ask detailed questions:
- Where does it hurt?
- When did it start?
- What makes it better or worse?
- Any recent injuries or changes in activity?
The physical exam involves hands-on testing. They’ll press on your back, buttocks, and legs to find tender spots. They’ll move your leg in different directions to see what reproduces your pain. Reflex testing, strength checks, and sensation tests help identify nerve problems.
Specific Tests for Piriformis Syndrome
Several clever maneuvers can unmask piriformis trouble. The test for piriformis syndrome vs sciatica includes these specific moves:
- The FAIR test puts your hip through Flexion, Adduction, and Internal Rotation. You lie on your side while the examiner moves your leg into these positions. If your buttock pain lights up, the piriformis muscle might be the culprit.
- The Pace maneuver tests the muscle’s strength. You sit and try to rotate your leg outward while the examiner resists the movement. Pain or weakness during this test suggests piriformis involvement.
- The Beatty test has you lie on your side and lift your top leg with the knee bent. Buttock pain during this position points toward piriformis irritation.
- The Freiberg maneuver involves forceful inward rotation of your hip while you’re lying down. This stretches the piriformis muscle and may reproduce symptoms if it’s the problem.
Imaging for piriformis syndrome mostly rules out other causes. MRI might show muscle swelling or nerve irritation, but there’s no single scan that definitively proves piriformis syndrome.

Specific Tests for Sciatica (Spinal Origin)
Spinal sciatica testing focuses on nerve root tension and structural problems.
- The Straight Leg Raise (SLR) test is a classic. You lie flat while the examiner lifts your straight leg. Pain shooting down your leg, especially between 30-70 degrees of elevation, suggests nerve root compression.
- The Slump test combines spinal flexion with leg extension to stress nerve roots. You sit and gradually bend your spine and neck while extending your leg. Leg pain reproduction indicates possible nerve root trouble.
- Imaging tells the real story for spinal sciatica. X-rays show bone problems and alignment issues. MRI is the gold standard for seeing disc herniations, spinal stenosis, and soft tissue problems. CT scans provide detailed bone images.
- Electromyography (EMG) and Nerve Conduction Studies (NCS) measure electrical activity in muscles and nerves. These tests identify nerve damage and pinpoint which specific nerves are affected.
The Importance of Ruling Out
Doctors usually investigate spinal causes first. Spinal problems can be more serious and may need different treatments, so ruling these out takes priority. This systematic approach ensures serious spinal conditions don’t get missed while chasing muscle-related diagnoses.
Finding the Right Treatment for Your Pain
Getting the right diagnosis matters because treatments for spinal sciatica and piriformis syndrome go in different directions.
Treatment for Sciatica (Spinal-related)
Spinal sciatica treatment often starts simply. Rest for a few days during bad flare-ups (but don’t stay in bed too long). Ice for the first 48 hours helps calm inflammation. Heat later might ease tight muscles.
- Medications play an important role early on. Anti-inflammatory drugs fight both pain and swelling. Muscle relaxants help if tight muscles add pressure on nerves.
- Physical therapy becomes your best tool, focusing on core strengthening to support your spine, posture work that fixes positions that pinch nerves, and specific exercises that help free trapped nerves. For example, many people find that gentle back extension exercises (like lying on your stomach and propping up on your elbows) help relieve disc-related sciatica.
- Stubborn cases might need nerve pain medications that work differently than regular pain pills. These target shooting, burning nerve pain specifically.
- Injections can deliver anti-inflammatory medicine right to irritated nerves. One shot might give months of relief.
- Surgery becomes an option when nothing else works and you have severe weakness or lose control of your bladder or bowels.
Treatment for Piriformis Syndrome
Piriformis syndrome treatment zeros in on muscle dysfunction and mechanical problems.
- Activity changes help immediately. Take breaks from sitting. Use cushions. Avoid movements that trigger symptoms.
- Physical therapy emphasizes specific stretches for the piriformis muscle. Various positions target different angles of the muscle. Hip flexor stretches address related tightness. Strengthening other hip muscles takes pressure off the overworked piriformis. For example, many runners find that regular stretching after workouts prevents piriformis flare-ups.
- Hands-on therapy like massage and dry needling can release muscle tension and trigger points. These techniques often provide quick relief and work well with stretching.
- Medications – anti-inflammatories and muscle relaxants – often work better for piriformis syndrome than for spinal sciatica.
- Injections can deliver steroids directly into the piriformis muscle to reduce inflammation. Botox injections help severe muscle spasms in tough cases.
- Lifestyle changes prevent recurrence. Ergonomic seating with good lumbar support reduces hip muscle strain. Proper shoes with arch support improve overall mechanics.
When to Seek Professional Help

Some symptoms need immediate attention:
- Sudden severe pain with leg weakness
- Loss of bladder or bowel control
- Numbness in your groin area
Get help soon if:
- Pain lasts more than 1-2 weeks despite self-care
- Pain gets progressively worse
- You develop a new weakness or numbness
Getting the right diagnosis changes everything. Knowing whether you have sciatica from piriformis syndrome or spine-related nerve compression ensures you get treatment that actually works for your specific problem.
Global Clinic offers a thorough evaluation using advanced techniques. Their specialists excel at telling these conditions apart and creating treatment plans that target your exact problem.
Ready to Reclaim Your Active Life?
Piriformis syndrome vs sciatica might feel similar, but they need completely different approaches. Spine-related sciatica comes from nerve compression in your back and needs different strategies than piriformis syndrome, which involves a tight muscle in your buttock. Knowing these differences puts you in control. Instead of accepting chronic pain or trying random treatments, accurate identification opens doors to solutions that actually work.
Recovery takes patience and often combines several approaches. Whether you’re dealing with spine compression or piriformis trouble, relief is absolutely possible with proper identification and personalized care. Don’t let confusion about piriformis syndrome vs sciatica keep you on the sidelines. Take charge by getting professional help when symptoms stick around. Your pain-free, active life is waiting.
FAQ
Can you have both piriformis syndrome and sciatica at the same time?
Yes. Spine nerve compression can happen alongside piriformis muscle problems. This creates overlapping symptoms that make diagnosis tricky. Professional evaluation helps sort out whether you have one condition or both.
Is walking good for piriformis syndrome or sciatica?
Walking often helps, both when done right. For piriformis syndrome, gentle walking keeps blood flowing and prevents stiffness. For sciatica, walking might help or hurt, depending on what’s pressing on your nerve. Start slow and stop if pain increases.
Why does my buttock hurt when I sit down?
Sitting pain usually points to piriformis syndrome since sitting directly pressures the muscle. However, some spine problems also cause buttock pain when sitting. The overall pain pattern helps tell them apart.
How long does recovery typically take for these conditions?
Piriformis syndrome often improves in 2-6 weeks with proper treatment. Stubborn cases might take months. Sciatica recovery depends on the cause – weeks for mild cases, months for severe spine problems needing surgery.
Can stretches really help piriformis syndrome?
Absolutely! Specific piriformis stretches can be incredibly effective. Regular stretching lengthens tight muscle fibers and reduces pressure on the nerve. Stretches work less well for spine-related sciatica, which needs the underlying spine problem addressed.


