Why Chronic Tendon Pain Doesn’t Have to Be Permanent
PRP for tendinopathy is a regenerative treatment that uses concentrated platelets from your own blood to promote natural tendon healing. Here’s what you need to know:
Quick Answer: Does PRP Work for Tendinopathy?
- What it is: A procedure that concentrates healing platelets from your blood (3-5x normal levels) and injects them into damaged tendons
- How it works: Growth factors in platelets stimulate collagen production, reduce inflammation, and support tissue repair
- Effectiveness: Studies show promising results for chronic Achilles, rotator cuff, and tennis elbow tendinopathy, particularly when combined with physical therapy
- Timeline: Most patients see gradual improvement over 3-6 months, not immediate relief
- Considerations: Typically requires 1-3 injections spaced 4-6 weeks apart; costs $500-$2,500 per session and is rarely covered by insurance
For the approximately 16.4 million Americans with tendon injuries each year, chronic pain is a frustrating reality. When traditional treatments like rest and physical therapy fail, the choice often seems to be between living with pain or undergoing surgery. That’s where regenerative medicine enters the picture.
Platelet-Rich Plasma (PRP) therapy offers a middle ground. Instead of masking symptoms, PRP aims to restart your body’s natural healing process by delivering concentrated growth factors directly to the injured tendon.
This guide will help you understand what tendinopathy is, how PRP works, what the research shows, and whether it might be right for you. As Practice Manager at Global Clinic with over 20 years of experience in regenerative medicine, I’ve helped countless patients explore PRP for tendinopathy. My goal is to help you make an informed decision.
Understanding Tendinopathy: More Than Just Inflammation
To understand how PRP for tendinopathy might help, it’s important to know what’s happening inside your tendon. It’s more complex than simple inflammation, which is why anti-inflammatory treatments often fall short.
The difference between tendinitis and tendinopathy matters. Tendinitis is acute inflammation from a sudden injury. Tendinopathy, however, is a chronic condition where the tendon’s healing process fails. Instead of repairing itself, the tendon’s structure degenerates. The strong, organized collagen fibers become jumbled and weak, like a fraying rope. The tendon gets stuck in a cycle of breaking down faster than it can rebuild, often with abnormal blood vessel growth and a shift to weaker types of collagen.
So what causes this breakdown? The most common culprit is repetitive strain or overuse, where the tendon can’t recover between activities. We see this constantly at Global Clinic in runners, tennis players, and office workers. The pattern is the same: repetitive movement without adequate recovery.
Aging also plays a role, as our tendons become less resilient and slower to repair. This doesn’t guarantee tendon pain, but it means they need more care.
Common symptoms that bring patients to our Northern Chicago clinic include:
- Pain with movement that worsens during or after activity.
- Localized tenderness directly over the affected tendon.
- Stiffness, especially in the morning or after periods of rest.
Understanding that tendinopathy involves failed healing helps explain why PRP for tendinopathy aims to restart and complete that stalled process, rather than just reducing inflammation. For a deeper look, you can explore current scientific opinions on tendinopathy from the research community.
How PRP Therapy Harnesses Your Body’s Healing Power
Now that we understand tendinopathy, let’s explore how PRP for tendinopathy works. This autologous treatment uses your own body’s resources to heal itself, concentrating your natural repair crew where it’s needed most.

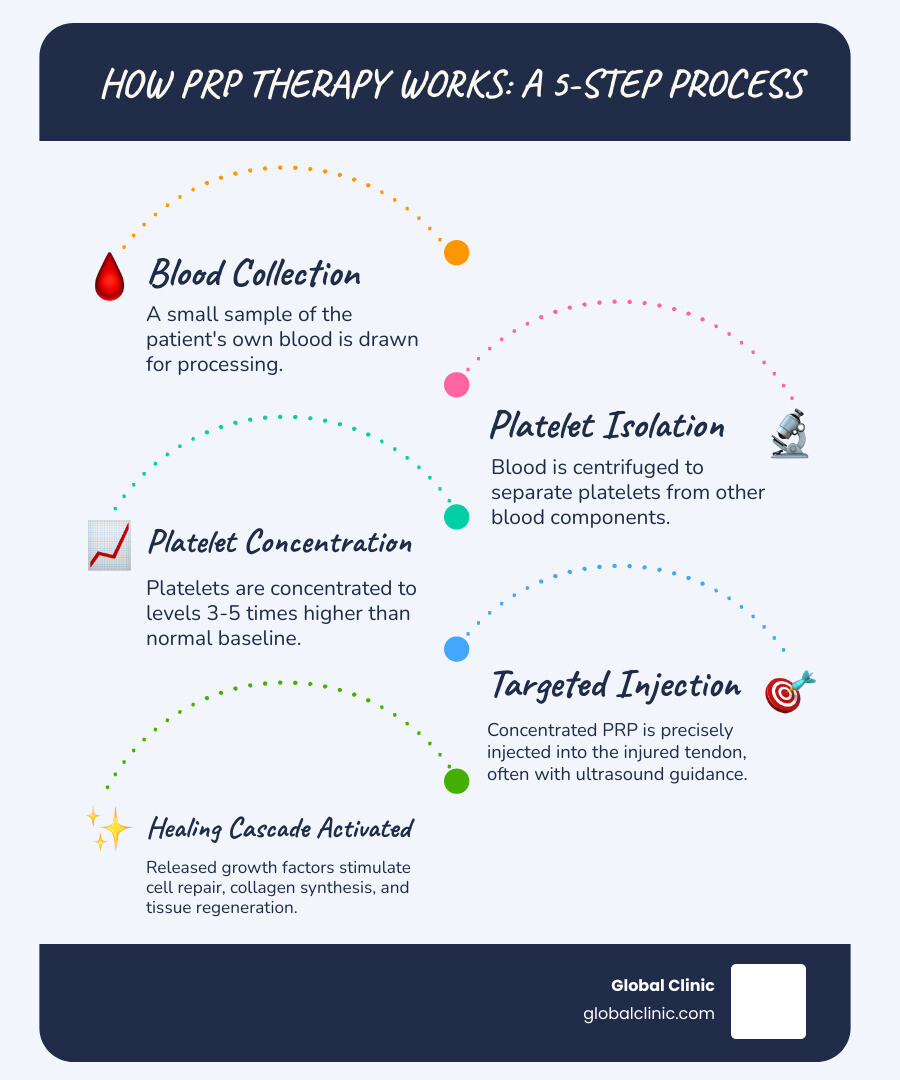
The process is straightforward and performed in our Northern Chicago clinic. We start with a simple blood draw from your arm. The blood is placed in a centrifuge, which spins at high speed to separate its components. The heavier red and white blood cells sink, leaving a golden plasma layer rich with platelets at the top. We extract this layer, which contains 3 to 5 times more platelets than normal blood. This is your Platelet-Rich Plasma.
When we inject this concentrated PRP into your damaged tendon, the platelets activate and release a cargo of growth factors. This kickstarts the healing cascade, signaling your tendon to shift from a degenerative state back into active repair mode.
The Science Behind PRP for Tendinopathy
The power of PRP for tendinopathy lies in the microscopic growth factors that promote tissue regeneration. These biological messengers don’t just mask pain—they help heal the tendon from the inside out.
These platelets release key growth factors like PDGF, TGF-β, VEGF, and IGF-1. Together, these proteins stimulate cell growth, promote the production of strong new collagen, improve blood supply, and help modulate the chronic inflammation that hinders healing. This coordinated effort helps remodel the damaged area, replacing degenerate tissue with a healthier, more functional tendon.
Research shows that PRP can improve collagen synthesis in damaged tendons, helping restore their structural integrity. For those interested in the detailed science, this comprehensive review of PRP mechanisms offers an in-depth look at how these processes unfold. At Global Clinic, we’ve seen these mechanisms translate into real improvements for patients with chronic tendon pain.
Clinical Applications: Where PRP for Tendinopathy Shows Promise
Patients at our Global Clinic in Northern Chicago often ask: “Will this work for my condition?” The good news is that PRP for tendinopathy has shown promising results for several chronic tendon issues that are often difficult to treat.
Successful treatment requires precision. We use ultrasound guidance to see the damaged tendon in real-time and deliver the concentrated platelets directly to the injury site. This ensures the PRP goes exactly where it’s needed. Our experience shows that PRP works best for chronic conditions that have persisted for months or years. Let’s look at the areas where research shows the most promise.
Rotator Cuff Tendinopathy
Rotator cuff tendinopathy causes shoulder pain and impaired mobility, often from repetitive overhead movements. Research on PRP for tendinopathy in the shoulder shows potential for functional improvement, especially when used as an adjunct to physical therapy. The PRP helps jumpstart healing while targeted exercises rebuild strength and proper movement.
Lateral Epicondylitis (Tennis Elbow)
This condition, common in carpenters and office workers, causes elbow pain and grip strength weakness. This is an area where research on PRP for tendinopathy is particularly strong. Multiple studies have shown superior long-term relief compared to corticosteroid injections, as PRP promotes actual healing rather than just temporarily reducing inflammation.
Patellar Tendinopathy (Jumper’s Knee)
Common in athletes, this condition causes knee pain just below the kneecap. For active individuals, a safe return to sport is crucial. Research on return-to-sport rates after PRP for patellar tendinopathy has been encouraging. Clinical findings on PRP for patellar tendinopathy suggest many athletes can return to their previous activity levels when PRP is combined with proper rehabilitation.
Achilles Tendinopathy
This overuse injury causes heel and ankle pain that can make walking uncomfortable. PRP is typically used for non-insertional tendinopathy (damage to the middle portion of the tendon). A systematic review of 406 patients showed significant improvements in pain and function scores. While the results are promising, researchers note that more high-quality studies are needed to fully establish its effectiveness compared to other treatments.
PRP vs. Traditional Treatments: A Comparative Look
If you have chronic tendon pain, you’ve likely tried various treatments. So where does PRP for tendinopathy fit in? The key difference is that most traditional treatments manage symptoms, while PRP aims to heal the damaged tissue.
Corticosteroid injections offer rapid but temporary relief by suppressing inflammation. They don’t heal the tendon, and repeated use can weaken the tissue, increasing rupture risk. In contrast, PRP for tendinopathy aims for long-term healing by delivering growth factors to repair the damage, with gradual improvement over months.
Over-the-counter NSAIDs like ibuprofen can reduce pain but come with risks like gastrointestinal issues with regular use. Like corticosteroids, they only provide temporary symptom relief without addressing the underlying tendon degeneration.
Physical therapy is one of the most valuable tools for tendinopathy, using exercises to rebuild the tendon’s capacity. However, some chronic cases don’t respond well to exercise alone. This is where PRP for tendinopathy can be a powerful complementary therapy. By jumpstarting healing at a cellular level, PRP creates a better environment for the tendon to respond to physical therapy.
At Global Clinic in Northern Chicago, we often see the best results when PRP is combined with a structured physical therapy program. The PRP initiates tissue repair, while physical therapy guides that repair toward renewed strength and function. Together, they can be remarkably effective for chronic tendon conditions.
The PRP Procedure: What to Expect
Knowing what to expect during a PRP for tendinopathy procedure can ease any concerns. The process is straightforward and designed for your comfort.
Your journey starts with a consultation at our Northern Chicago facility to determine if PRP is right for you. Before the procedure, we’ll provide pre-procedure guidelines. You’ll need to stop taking corticosteroid medications 2-3 weeks before and NSAIDs about one week prior. We also ask you to stay well-hydrated.
The Three-Step Injection Process
The procedure itself takes about 45 to 90 minutes.
Step 1: Blood Draw. We draw a small amount of blood from your arm, just like a routine lab test.
Step 2: Blood Processing. We use a centrifuge to spin your blood, separating and concentrating the platelets to create a solution 3 to 5 times richer in healing growth factors.
Step 3: Guided Injection. After cleaning the area, we use ultrasound guidance to inject the PRP directly into the damaged tendon tissue. This real-time imaging ensures precise delivery for optimal results.

Is PRP for Tendinopathy Right for You?
PRP is not for everyone. You might be an excellent candidate if you’ve had chronic tendon pain for over three months and conservative treatments haven’t provided lasting relief. It’s a great option for those hoping to avoid surgery.
However, PRP is not recommended if you have certain contraindications, which we will review with you. These include:
- Blood disorders affecting platelet function
- Active infections
- Certain types of cancer
- Pregnancy
Safety, Risks, and Recovery
Because PRP uses your own blood, the risk of allergic reaction or disease transmission is virtually zero. The most common side effects are temporary pain, swelling, or bruising at the injection site, which usually fade within a few days.
Recovery begins immediately. Expect some normal swelling and discomfort, managed with rest and cold compresses. It’s crucial to avoid anti-inflammatory medications (like ibuprofen) for at least four weeks, as they can hinder the healing process. We may recommend a temporary brace or sling. After about four to five weeks, you’ll begin a physical therapy program to rebuild strength. This combination of PRP and targeted exercise is key to a successful, long-term outcome.
Frequently Asked Questions about PRP for Tendinopathy
At Global Clinic, we’ve answered thousands of questions about PRP for tendinopathy over the last two decades. Here are answers to the most common ones.
How long does it take for PRP to work for tendinopathy?
PRP is not an instant fix. You may experience an initial inflammatory response for a week or two, which is a normal part of the healing process. Most patients see gradual improvement over 3 to 6 months as the tissue regenerates. The timeline varies based on the individual, condition severity, and the specific tendon treated. The goal is lasting tissue repair, not a temporary solution.
Is the PRP injection painful?
We use a local anesthetic to numb the area, so most patients feel only pressure or a dull ache during the injection. Post-injection soreness and mild swelling are common for a few days and are a sign that the healing process is starting. This discomfort is typically manageable with cold compresses and approved pain relievers (avoiding NSAIDs).
How many PRP injections are needed for tendinopathy?
There is no one-size-fits-all answer. We create personalized treatment plans at Global Clinic. Typically, we recommend a series of 1 to 3 injections, spaced about 4 to 6 weeks apart. The number depends on the severity of your condition and how your body responds to the initial treatment. We monitor your progress and adjust the plan as needed, never recommending more treatments than necessary.
Challenges, Limitations, and Future Directions
While PRP for tendinopathy is promising, it’s important to be realistic about its current state. As a treatment that has evolved over the last two decades, it still has some challenges.

Key challenges include the lack of standardization in PRP preparation and administration protocols, which can lead to variable results. The distinction between leukocyte-rich (L-PRP) and leukocyte-poor (P-PRP) preparations, for example, can significantly impact outcomes. This variability makes it difficult to compare study results and establish universal guidelines.
Another major hurdle is the cost consideration. Because most insurance companies still consider PRP investigational, patients often pay out-of-pocket. Prices typically range from $500 to $2,500 per injection, and a full treatment course may require multiple sessions. This can be a significant barrier for many.
Despite these limitations, the future of PRP for tendinopathy is bright. Researchers are working to optimize PRP formulations for specific conditions, moving toward customized preparations. There is also growing interest in combination therapies, such as pairing PRP with other regenerative treatments or highly specific physical therapy protocols to amplify the benefits.
Perhaps most importantly, the medical community is working to identify which patients will respond best to PRP, which will allow for truly personalized regenerative medicine. As larger, more rigorous clinical trials with standardized protocols are completed, we expect to see more definitive guidelines and, hopefully, broader insurance coverage.
At Global Clinic, we stay at the forefront of these developments, continuously updating our protocols based on the latest evidence to deliver the best possible outcomes for our patients in Northern Chicago.
Conclusion: Taking the Next Step Towards Tendon Health
Chronic tendon pain can be frustrating and limiting, but you have options beyond traditional treatments that may not have worked. PRP for tendinopathy represents a different approach, one that works with your body to heal from within.
By concentrating your blood’s natural growth factors and delivering them to the site of injury, PRP aims to restart a stalled healing process. We’ve seen how it can stimulate collagen synthesis and promote tissue regeneration for conditions like Achilles tendinopathy, rotator cuff issues, and tennis elbow. Unlike corticosteroids or NSAIDs that focus on symptoms, PRP targets the underlying problem to create lasting change.
PRP is not a miracle cure. Healing takes time—typically three to six months—and results vary. However, for many patients who have exhausted conservative options and wish to avoid surgery, PRP for tendinopathy offers a valuable path forward.
At Global Clinic, we have spent over 20 years providing personalized, innovative care to patients across Northern Chicago. We understand that your pain affects your entire life, and we take the time to develop a treatment plan custom to your specific needs and goals.
If you’re ready to explore whether PRP therapy is right for you, we’re here to help. Your journey toward improved tendon health could start with a simple conversation.