A Minimally Invasive Solution for Joint Pain
Joint injection therapy is a minimally invasive treatment that delivers medication directly into painful joints to reduce inflammation, manage pain, and improve mobility. This procedure offers relief for millions of Americans suffering from arthritis, acute injuries, and general wear and tear.
Quick Overview of Joint Injection Therapy:
- What it is: Direct injection of medication into joints or surrounding tissues
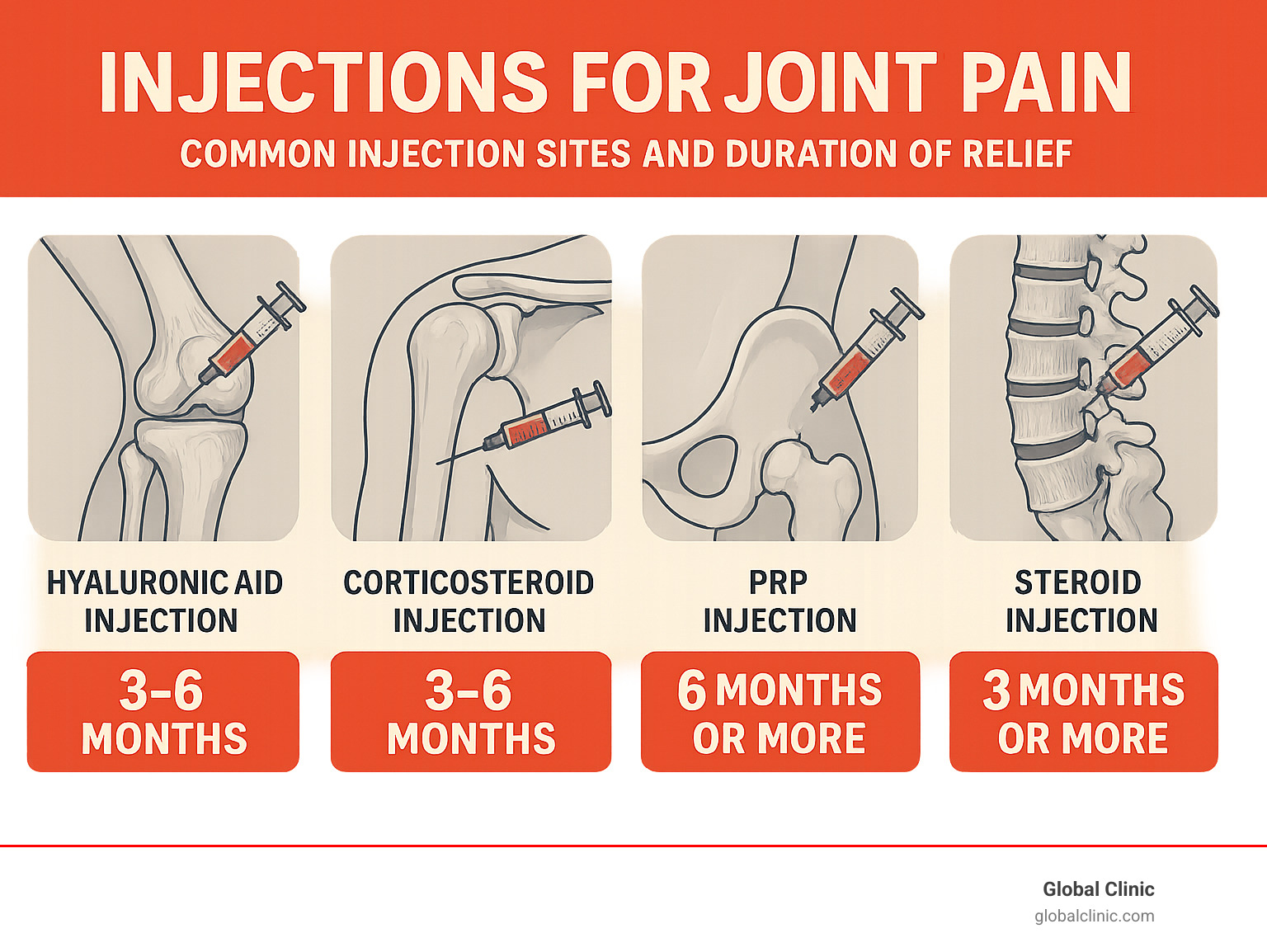
- Types: Corticosteroids, hyaluronic acid, platelet-rich plasma (PRP)
- Duration: Relief typically lasts 3-6 months or more depending on injection type
- Procedure time: 15-30 minutes in an outpatient setting
- Recovery: Most patients resume normal activity within 1-2 days
- Purpose: Bridge to physical therapy and long-term pain management
More than 50 million Americans suffer from arthritis-related joint pain, with millions more experiencing discomfort from injuries and wear and tear. Joint injections target the source of pain, offering a non-surgical alternative when rest, exercise, and medication haven’t provided enough relief.
The procedure provides sufficient pain relief to enable patients to engage in physical therapy and other rehabilitation. Whether you’re dealing with knee osteoarthritis, shoulder bursitis, or chronic back pain, joint injections can offer significant symptom improvement while you address the underlying causes.
I’m Ana Vinikov, Practice Manager at Global Pain & Spine Clinic. Our multidisciplinary team has over 20 years of experience in joint injection therapy and comprehensive pain management, helping thousands in the Chicago area find lasting relief with personalized treatment plans.
Joint injection therapy helpful reading:
Understanding the Types of Joint Injection Therapy
Joint injection therapy offers several approaches designed to target pain and inflammation. At Global Clinic, we use different types of injections depending on your specific needs. To learn more about how joint injections are administered and why, see this overview of intra-articular injections.
Corticosteroid Injections
Corticosteroid injections, or “cortisone shots,” are a reliable way to quickly reduce inflammation and pain. We combine a powerful anti-inflammatory medication with a local anesthetic. The anesthetic provides immediate relief, while the corticosteroid reduces the underlying inflammation.
These injections are effective for osteoarthritis, tendinitis, bursitis, rheumatoid arthritis, and gout flare-ups. Most patients experience relief for 3-6 months. To protect long-term joint health and prevent potential weakening of cartilage and tendons, we limit corticosteroid injections to 2-3 per year per joint.
Hyaluronic Acid (HA) Injections
Hyaluronic acid injections, also known as viscosupplementation, supplement your joint’s natural lubrication. Healthy joints contain synovial fluid that helps them move smoothly. In arthritic joints, this fluid breaks down. HA injections restore this lubricating quality, acting as a natural joint fluid mimic to cushion the joint.
These injections are primarily used for knee arthritis when other treatments have failed. Patients typically feel the benefits in 4-6 weeks, and relief often lasts 6-12 months, making them a good option for longer-lasting results. For comprehensive strategies on managing knee discomfort, check out our guide: More info about relieving knee pain.
Regenerative Medicine Injections
Regenerative medicine injections aim to help the body heal itself.
Platelet-Rich Plasma (PRP) is a popular option where we concentrate platelets from your own blood and inject them into the joint. These platelets contain healing factors from your own blood that reduce inflammation and encourage tissue repair.

Autologous Conditioned Serum (ACS) is another option that uses specially prepared blood to boost anti-inflammatory properties, with research showing relief can last up to two years with physical therapy.
These treatments work by stimulating natural healing, so full benefits may take 2-3 months to appear, but the results can be very long-lasting.
Want to learn more about how PRP might help you? Visit our detailed guide: PRP Injections.
The Joint Injection Procedure: What to Expect
If you’re considering joint injection therapy, the process is straightforward. We guide you through each step, from consultation to recovery.
Preparing for Your Injection
Thorough preparation is key to a successful outcome. Your journey begins with an initial consultation to discuss your pain, medical history, and how your condition affects your life. A physical examination, including range-of-motion tests, helps us pinpoint the source of your pain.
We may use diagnostic imaging like X-rays or an MRI to get a clear view of the joint and guide the injection. It’s crucial to discuss your medications, as you may need to temporarily stop blood thinners before the procedure. Please also inform us if you’ve had a recent fever, as this may require rescheduling.
During the Procedure
The procedure takes place in our outpatient facility. We begin by cleaning the injection site with an antiseptic. A local anesthetic is then applied to numb the area, minimizing discomfort.
For precision, we use image guidance for accuracy, such as fluoroscopy or ultrasound. Ultrasound-guided interventions are especially effective for visualizing soft tissues and ensuring perfect placement. The entire appointment, including preparation, typically takes 15-30 minutes, with the injection itself lasting only a few minutes.
Recovery and Aftercare
After a short monitoring period (15-30 minutes), you can go home. Following our aftercare guidelines is crucial for the best results.
- Rest for 24-48 hours: Avoid heavy lifting or excessive strain on the injected joint.
- Apply ice: Use an ice pack for 15-20 minutes at a time to reduce any mild soreness or swelling.
- Avoid strenuous activity: Postpone gym sessions, heavy chores, and hot tubs for at least two days.
- Potential “steroid flare”: A temporary increase in pain for up to two days is normal for corticosteroid injections and resolves on its own.
- Monitor for infection signs: Though rare, contact us immediately if you notice increasing pain, redness, swelling, or fever.
A gradual return to activity is usually possible within a couple of days. Combining injections with physical therapy is often recommended to strengthen the joint and achieve lasting relief.
Evaluating Joint Injections as a Treatment Option
Deciding if joint injection therapy is right for you involves understanding candidacy, the conditions it treats, and how it fits into your overall pain management plan.
Conditions Treated and Candidacy for Joint Injection Therapy
Joint injection therapy is effective for many conditions, especially when conservative treatments have failed. We commonly treat:
- Osteoarthritis (“wear and tear” arthritis)
- Rheumatoid arthritis (autoimmune inflammation)
- Gout (sudden, intense flare-ups)
- Bursitis and tendinitis
- Acute injuries like sprains
- Chronic back pain from facet or sacroiliac joints
Ideal candidates are those with chronic pain impacting their daily life. Injections offer a non-surgical alternative that can delay or prevent surgery and serve as a bridge to physical therapy by providing enough relief to engage in rehabilitative exercises. If you’re living with knee pain, our comprehensive approach can help. Explore living comfortably with knee arthritis.
Benefits and Risks of Joint Injection Therapy
Benefits of joint injection therapy include:
- Significant pain relief and reduced inflammation.
- Improved mobility and function.
- Minimally invasive procedure with minimal downtime.
- Targeted treatment with fewer systemic side effects than oral medication.
- Diagnostic value in pinpointing the source of pain.
Potential risks are low but include infection, bleeding, bruising, and rare nerve damage. A temporary pain flare can occur after corticosteroid injections. With repeated corticosteroid use, there is a risk of cartilage deterioration or tendon weakening, which is why we limit their frequency. We will discuss all benefits and risks with you thoroughly.
| Injection Type | Typical Duration of Relief |
|---|---|
| Corticosteroids | Weeks to a few months (3-6 months common for chronic pain) |
| Hyaluronic Acid (HA) | 6 to 12 months |
| Platelet-Rich Plasma (PRP) | Months to years |
| Autologous Conditioned Serum (ACS) | Up to two years (with physical therapy) |
Cost, Insurance, and Comparison to Other Treatments
Corticosteroid and hyaluronic acid injections are typically covered by medical insurance, though pre-authorization may be required. Regenerative medicine injections like PRP and ACS are often considered experimental by insurance, which can lead to out-of-pocket costs. We will discuss all costs with you upfront.
Compared to other treatments:
- Physical Therapy: Injections can provide the pain relief needed to participate more effectively in PT, like physical therapy after a car accident.
- Oral Medications: Injections are targeted, avoiding the systemic side effects of oral drugs.
- Surgery: Injections are a less invasive alternative that can delay or prevent the need for surgery.
- Radiofrequency Ablation (RFA): This is another minimally invasive option for specific types of chronic pain, offering long-lasting relief.
Frequently Asked Questions about Joint Injections
It’s natural to have questions about joint injection therapy. Here are answers to some of the most common ones we hear.
How long do joint injections last?
The duration of relief depends on the type of joint injection therapy:
- Corticosteroid injections: Relief typically lasts for weeks to a few months (commonly 3-6 months).
- Hyaluronic acid injections: These tend to last longer, usually 6 to 12 months.
- Regenerative medicine (PRP, ACS): Results can last from months to years.
Your individual results will vary based on your condition’s severity, your body’s response, and your participation in rehabilitation.
Are joint injections painful?
We take every measure to make the procedure as comfortable as possible. A local anesthetic is used to numb the area, so most patients only feel a brief sting and some pressure. Post-injection soreness for a day or two is normal and can be managed with ice.
Some patients may experience a temporary “steroid flare,” or increased pain for up to two days, which is a normal response that resolves on its own. Most patients find the temporary discomfort is minor compared to the pain relief they achieve.
How many joint injections can I have?
The number of injections depends on the type and your individual needs.
- Corticosteroid injections: We limit these to two or three per year per joint to protect cartilage and tendons from potential long-term damage.
- Hyaluronic acid and PRP injections: These do not have the same risks and can be repeated more frequently. HA injections are often repeated every 6-12 months, while PRP is typically given in a series.
We will create a personalized treatment plan that prioritizes your long-term joint health and fits into your broader pain management strategy.
Conclusion: Taking the Next Step in Your Pain Management Journey
Living with joint pain doesn’t have to be your reality. Joint injection therapy is a remarkable pain management tool, offering a minimally invasive solution when other treatments fall short. From fast-acting corticosteroids to long-lasting regenerative medicine, these therapies can restore mobility and comfort.
More importantly, they create a window of opportunity for you to engage in physical therapy, strengthening your joints and addressing the root causes of your pain for lasting improvement.
At Global Clinic, we have over 20 years of experience helping patients in Northern Chicago communities like Arlington Heights, Schaumburg, and Glenview. We create personalized treatment plans custom to your unique condition and goals. While joint injection therapy is highly effective, some patients may benefit from other advanced options. For chronic back and neck pain, Radiofrequency Ablation (RFA): The Newest Pain Control Method can offer even longer-lasting control.
Your pain management journey is personal, but you don’t have to steer it alone. Our multidisciplinary team is here to guide you. Taking the first step toward relief begins with a conversation about what’s possible for you.


